qMIDS, the world’s first rapid oral cancer test, has been developed by Queen Mary University of London and an international team of researchers. It has the potential to relieve pressure on the NHS and may improve the early detection of oral cancer.
Saving Faces has supported researchers at Queen Mary University of London who have developed the world’s first PCR test for mouth cancer. The test has now been proved with patients from China, India and the UK, with the results published in the international journal, Cancers. The inventor, Dr Muy-Teck Teh, named the test the Quantitative Malignant Index Diagnosis System (qMIDS).
qMIDS diagnostic accuracy would mean that 90% of low-risk patients could be discharged from hospital to go back to their dentist or GP for review. Or they might be tested in the dentist’s surgery and only referred to secondary care if they were high risk. High-risk cases could also be detected in the pre-cancer period and treated definitively, thereby saving the patient’s life with minor surgery, better cure rates and quality of life, as well as a huge reduction in health service costs.
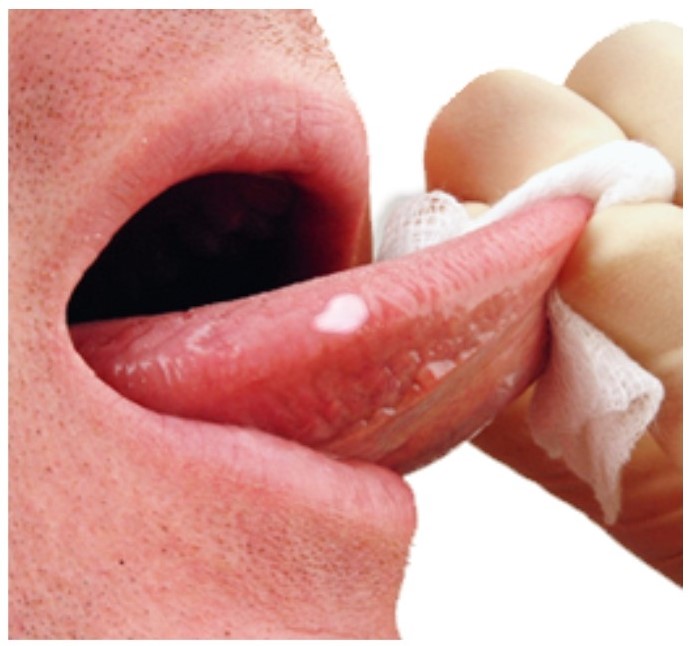
The test process is largely automated, removing the need for expensive pathologists. There’s also no need for invasive biopsies. The tests can be carried out on multiple sites when patients have lesions affecting large areas throughout the mouth.
Co-study lead, Professor Iain Hutchison, stated: “qMIDS dramatically improves our management of mouth cancer and its pre-cancerous state, saving lives and healthcare costs. Surgeons and dentists anywhere in the world can use this test for minimally invasive tissue samples because all it needs is a PCR machine and the technician who operates it.
“qMIDS will help us identify patients with pre-malignancies that will never transform to cancer, so they can be reassured and discharged from hospital review. Patients with high-risk premalignancy can have minor surgery to remove the lesion before it has transformed to cancer, thereby curing the patient and saving them major surgery, which in turn reduces health service costs. It is a powerful tool especially when used in conjunction with conventional histopathology assessment.”
Read full journal article here
Read news coverage here